
ST2 is a cardiac biomarker, which is used to evaluate the prognosis in patients with acute coronary syndrome and chronic heart failure. It belongs to the IL-1 (interleukin-1) receptor family. ST2 has 2 isoforms: soluble ST2 (sST2) and ST2 bound to a cell membrane (ST2L). When the level of soluble ST2 is low, the ligand of ST2, IL-33, binds to ST2L, and this has a cardioprotective effect. However, when the amount of sST2 is increased, it competitively binds to IL-33. As a result, IL-33 cannot bind to ST2L for cardioprotective signaling. Research has shown, that increasing the amount of soluble isoform of ST2 causes reducing of cardiac function, death of cells and myocardium fibrosis.
When is the test ordered?
ST2 levels can be measured to evaluate risks of hospitalization and mortality in patients with chronic heart failure. ST2 is used as a dichotomous marker, which can identify high and low risk patients. Measuring both ST2 and NT-proBNP can be helpful to more accurately evaluate the prognosis; each of these tests is an independent marker and the unique information received from them complements each other.
ST2 is not used to diagnose heart failure. It is ordered in only patients with diagnosed chronic heart failure.
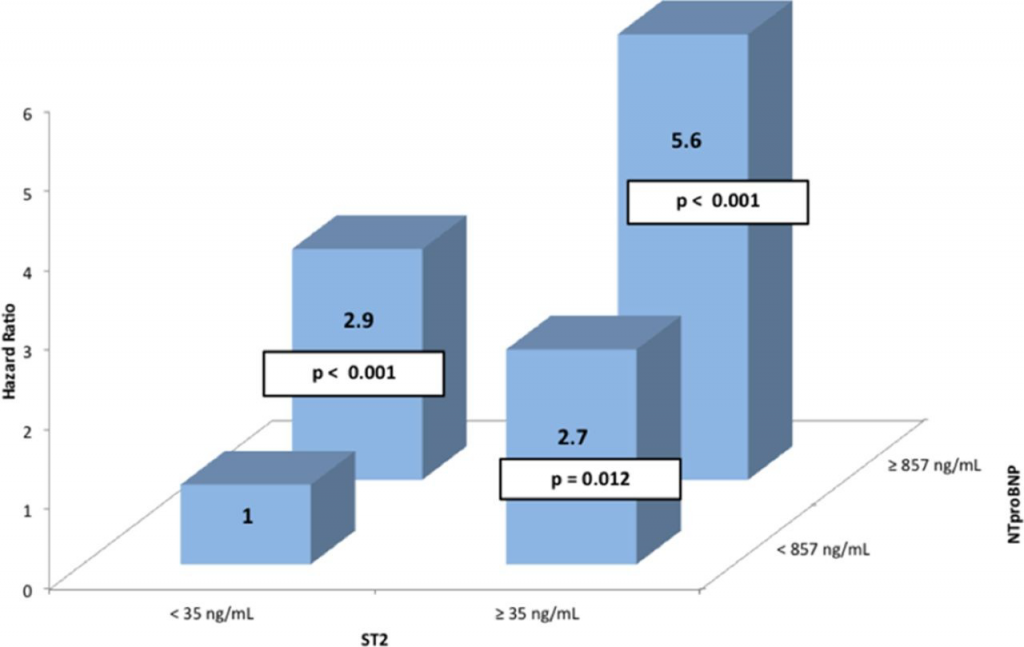
(the source of the diagram: http://circheartfailure.ahajournals.org/content/6/6/1172.full)
How is this test performed?
This test measures the amount of soluble ST2 in the serum. A blood sample is taken from a vein. Prior to the test, it is essential to first consult with a doctor and get the exact instructions about any preparation needed.
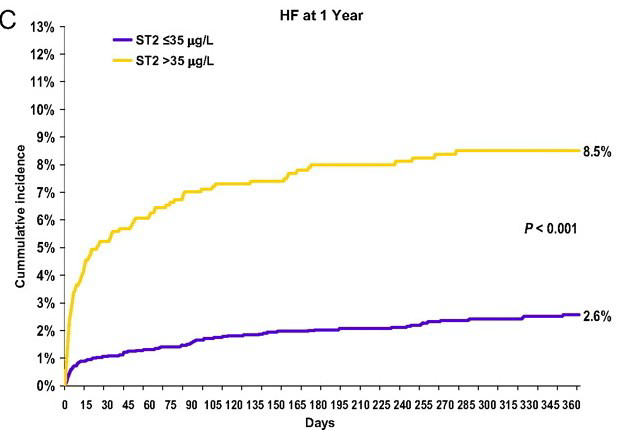
The test results should be interpreted by a doctor. Research showed that ST2 level at 35 ng/ml is the value that can be used to divide patients into higher and lower risk groups. Patients with ST2 level below 35 ng/ml, have better prognosis compared to patients with higher amounts of ST2. Serum level of ST2 above 35 ng/ml is associated with increased risk of hospitalization and mortality.
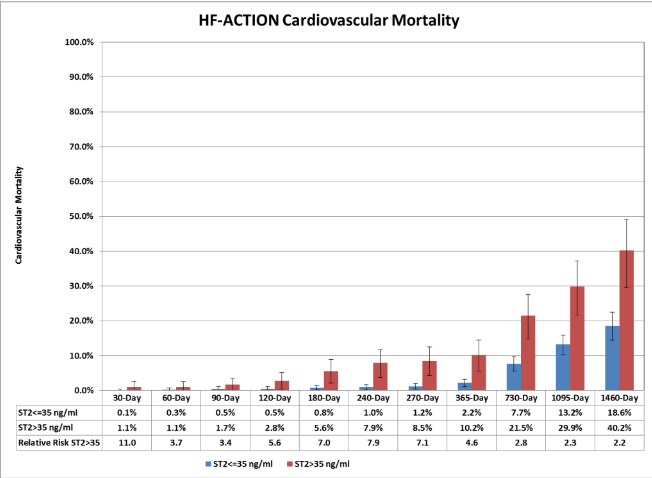
the source of the diagram: http://clinchem.aaccjnls.org/content/58/1/257.full
sources:
http://www.ncbi.nlm.nih.gov/pubmed/18827826
http://circ.ahajournals.org/content/107/5/721.full
